For legal professionals, compliance officers, and administrative staff, the act of sharing Protected Health Information (PHI) is a high-stakes legal exercise. Every request for a patient’s medical chart, diagnostic result, or treatment summary requires a valid, legally compliant, and meticulously executed Medical Records Release Form.
In the United States, this single document serves as the firewall for the Health Insurance Portability and Accountability Act (HIPAA) and its numerous state-level variations. A deficient or outdated release form can instantly torpedo critical personal injury litigation, stall an insurance investigation, or expose a Covered Entity to massive federal fines and litigation.
Far too many organizations still rely on generic, unverified medical release form templates—a precarious one-size-fits-all approach that ignores the dynamic nature of legal mandates.
This comprehensive guide is authored for legal and compliance experts, providing an authoritative breakdown of the legal, practical, and technical requirements for the Authorization to Use or Disclose PHI. We will dissect the mandatory components, provide real-world legal use cases, and demonstrate how Wansom’s secure, AI-powered collaborative workspace can automate the creation of audit-ready, state-compliant forms, turning a common liability into a core procedural strength.
Wansom’s Medical Release Form Template: Compliance at the Core
Wansom’s Medical Records Release Form Template is not a static document; it is a dynamic, AI-guided blueprint engineered for legal certainty.
-
Audit-Ready Compliance: The template meets all six mandatory elements of HIPAA (45 CFR § 164.508) and is dynamically adjusted to comply with the most stringent state-specific requirements.
-
Targeted Sensitivity: Includes specific, legally distinct sections and mandatory check-boxes to address the disclosure of highly sensitive PHI (e.g., HIV/AIDS status, mental health notes, 42 CFR Part 2 Substance Use Disorder treatment records).
-
AI-Guided Customization: Use Wansom's integrated AI assistant to effortlessly adjust the scope, duration, and parties of the form, ensuring it perfectly matches the unique needs of a specific litigation matter or insurance claim.
Related to Blog: The Cost of Non-Compliance: A Legal Analysis of Recent HIPAA Fines
What is a Medical Release Form?
A medical release form (often referred to as an Authorization to Release Medical Information or a HIPAA Authorization) is a critical legal document that provides the patient's express, written permission for a healthcare provider (the Disclosing Party) to share their Protected Health Information (PHI) with a specified third party (the Recipient).
This mechanism is the cornerstone of patient privacy protection. While routine information sharing occurs constantly to facilitate safe and effective medical care, providers must obtain a release form whenever the disclosure moves beyond the patient's reasonable expectation of shared information.
In the US, these forms are fundamentally rooted in compliance with the Health Insurance Portability and Accountability Act (HIPAA). In contrast, many international jurisdictions, such as Australia and the UK, rely heavily on common law duties of confidentiality alongside specific regulations like the GDPR (UK) and the Australian Privacy Principles (APP). However, regardless of the jurisdiction, the core legal principle remains the same: the patient must formally authorize the disclosure of their private medical records outside of routine care.
Related to Blog: International Data Privacy Laws: GDPR vs. HIPAA for Global Legal Teams
When to Use a Medical Release Form
Clinicians are permitted to legally share a patient’s information in many situations involving the routine delivery of care (known as Treatment, Payment, and Healthcare Operations, or TPO). For example, a surgeon can share operative notes with the post-operative nurse without needing a formal release.
However, the legal imperative to protect patient privacy requires a signed Medical Records Release Form for situations where there is no reasonable expectation on the patient’s behalf that their information would be shared.
To accurately determine when a release form is mandatory, legal teams must first establish the legal framework governing PHI handling.
Medical Records Release Forms: Privacy and Confidentiality 101
While often used interchangeably in lay language, Privacy and Confidentiality have distinct legal meanings that define the scope of a release form's necessity.
Privacy
Privacy refers to the laws and regulations that govern how patient information is collected, handled, used, and accessed. These laws mandate security requirements, restrict the use of data for marketing, and establish patient rights over their records.
-
US: Governed by HIPAA (The Privacy Rule).
-
UK/EU: Governed by the General Data Protection Regulation (GDPR).
-
Australia: Governed by the Australian Privacy Principles (APP).
Confidentiality
Confidentiality describes the healthcare provider’s ethical and professional obligation to protect information disclosed to them by the patient while delivering care. It applies both to formal written records and informal conversations.
In the US and UK, while HIPAA/GDPR provides the statutory framework, the common law duty of confidentiality and professional codes of practice also heavily influence a provider's obligation not to disclose PHI without authorization.
Understanding HIPAA
HIPAA provides the definitive legal framework in the United States, offering clear definitions of the information that must be protected and the entities responsible for that protection.
What is Protected Health Information (PHI)?
According to the HIPAA Privacy Rule, Protected Health Information (PHI) encompasses any individually identifiable health information that relates to:
-
The individual's past, present, or future physical or mental health or condition.
-
The provision of health care to the individual.
-
The past, present, or future payment for the provision of health care to the individual.
Crucially, PHI is not just clinical details; it includes information that can be used to identify an individual, such as demographics, dates (except year), specific geographic identifiers, and unique identifiers (Social Security Numbers, medical record numbers). The entire purpose of a Medical Release Form is to create a legally sanctioned exception to the non-disclosure rule for PHI.
Permitted Uses and Disclosures of PHI
Clinicians and Covered Entities are permitted to use and disclose PHI without an individual’s authorization for specific, necessary purposes:
-
Treatment, Payment, and Healthcare Operations (TPO): This is the core exception, covering the routine coordination of care, billing the insurance company, and quality assessment activities.
-
Public Interest and Benefit Activities: Disclosures required by law (e.g., subpoena, mandatory infectious disease reporting), to prevent serious and imminent threat to health or safety, or for workers’ compensation claims.
-
To the Individual: Giving the patient access to their own PHI.
Outside of these strictly defined permitted disclosures, a signed Authorization (Medical Release Form) is mandatory before sharing PHI. Furthermore, in all permitted instances, the Minimum Necessary Rule applies: only the minimum amount of information required to fulfill the request should be provided.
Related to Blog: The Minimum Necessary Rule: Practical Application in Legal and Compliance
Medical Records Release Form Scenarios
Knowing when to require a signed authorization is the difference between legal compliance and a major violation. The following scenarios illustrate when a Medical Release Form is generally required versus when it is not.
A Medical Release Form is Generally NOT Required for:
-
Treatment Purposes: Information shared among healthcare providers or specialists directly involved in a patient’s concurrent care (e.g., an attending physician sharing notes with a consulting specialist).
-
Payment Operations: Sharing information with a health plan or insurance company solely for the purpose of submitting claims and obtaining reimbursement.
-
Healthcare Operations: Using anonymized or de-identified patient data for internal quality assessment, peer review, audits, or administrative functions.
-
Emergencies: Disclosing information to facilitate immediate, life-saving care when obtaining authorization would cause a harmful delay.
A Medical Release Form IS Usually Needed Before:
-
Third-Party Disclosure: Sharing records with entities not directly involved in TPO, such as employers (outside of workers' compensation), life insurance companies, or attorneys (for litigation or legal counsel).
-
Family Disclosure (Non-Representative): Releasing information to family members (e.g., spouse, parent, adult child) who are not designated as the patient's legal representative (Healthcare Power of Attorney) or guardian.
-
Sensitive Information: Disclosing specially protected categories of information, which often require separate, explicit patient initials on the form. This includes:
-
Substance Use Disorder (SUD) records (governed by the more restrictive 42 CFR Part 2).
-
Mental health psychotherapy notes.
-
HIV/AIDS status or genetic information.
-
-
Commercial/Non-TPO Use: Using patient information for marketing, fundraising, or research purposes not covered under a waiver granted by an Institutional Review Board (IRB).
Best Practice for Legal Teams: When the purpose of the disclosure is litigation, insurance evaluation, or any non-routine administrative function, always insist on a valid, complete, and signed Medical Records Release Form.
Related to Blog: Navigating 42 CFR Part 2: Substance Abuse Records and Legal Discovery
Challenges with Medical Release Forms
Even with a template, the manual administration of release forms is fraught with challenges that introduce legal risk, administrative friction, and time delays.
Breaching Confidentiality Due to Risk
Clinicians frequently face the ethical and legal dilemma of a Duty to Protect principle (e.g., Tarasoff v. Regents of University of California). This stipulates that if a patient poses a serious and imminent threat of violence to a potential victim, the clinician may be required to breach confidentiality to warn the victim or notify law enforcement.
-
The Challenge: The decision to breach is complex, requiring precise judgment and immediate action.
-
The Solution: Legal guidance on the Duty to Protect must be seamlessly integrated into practice protocols. Wansom’s platform ensures that all documentation generated—whether a referral or an authorization form—is contextualized against legal precedent, allowing legal counsel to quickly audit the compliance record when risk disclosure occurs.
Release of Information Outside of Healthcare Systems
Requests from entities like social services, educational institutions, or legal representatives are routine but necessitate strict adherence to disclosure protocols. The manual process often involves unnecessary back-and-forth communication to verify the request's legitimacy.
Deciding What Information to Send (The Minimum Necessary Rule)
The Minimum Necessary Rule is often violated in practice. A generic request for "all records" should not lead to the release of the patient's entire chart, especially if only a specific date range or injury is relevant.
-
The Challenge: Staff must manually review lengthy records to redact non-essential information and ensure sensitive data is not accidentally included without explicit authorization.
-
The Wansom Advantage: Wansom's AI is specifically designed for content synthesis. For legal teams, the AI can ingest the full medical record and, based on the specific scope defined in the Wansom template (e.g., "lumbar spine injury records between 2023-2024"), generate a redacted, compliant summary for disclosure, ensuring the minimum necessary information is always provided. This drastically cuts manual review time and enhances compliance integrity far beyond simple form-filling solutions.
Time and Cost of Releasing Information
The administrative burden of processing forms and preparing compliant records for disclosure is enormous. The steps include: verification, obtaining patient signature, locating records, manual review/redaction, and secure transmission. This administrative drag is a major hidden cost for legal and healthcare firms alike.
The transition from manual processes to secure, AI-powered automation is the only sustainable way to manage the escalating volume and complexity of PHI requests.
Related to Blog: Reducing Legal Practice Overhead: The Economics of Document Automation
Essential Parts of a Release of Medical Records Form
To be legally enforceable and HIPAA compliant, a Medical Records Release Form must be viewed as a formal contract of consent. The following components are essential and must be clearly defined in your firm's template:
-
Patient Information: Full legal name, date of birth, address, and Medical Record Number (MRN). This guarantees correct patient identification.
-
Specific Description of Information: Details the exact types of records being sought (e.g., "operative reports," "physical therapy notes") and the specific dates of service or date ranges.
-
Specific Disclosing Party: Clearly names the individual physician, clinic, or hospital authorized to release the records.
-
Specific Recipient Information: Names the authorized person or entity (e.g., "Law Office of J. Smith," "Acme Insurance Company") who may receive and handle the information.
-
Statement of Purpose: A clear, concise statement outlining why the records are being requested (e.g., "For litigation purposes in the matter of Doe v. Roe," "To determine eligibility for disability benefits").
-
Expiration Clause: A date or specific event upon which the authorization expires. This is mandatory; authorizations cannot be indefinite.
-
Revocation Clause: A clear statement informing the patient of their right to revoke the authorization at any time in writing, along with instructions on how to do so.
-
Sensitive Information Waiver: Checkboxes and initial spaces for the patient to explicitly authorize the release of highly protected PHI (e.g., Mental Health, SUD, HIV).
-
Redisclosure Warning: A statement warning the patient that once the PHI is released to the recipient (e.g., a law firm), it may no longer be protected by HIPAA and could be redisclosed.
-
Authorization Signature and Date: The signed and dated authorization from the patient or their qualified Personal Representative.
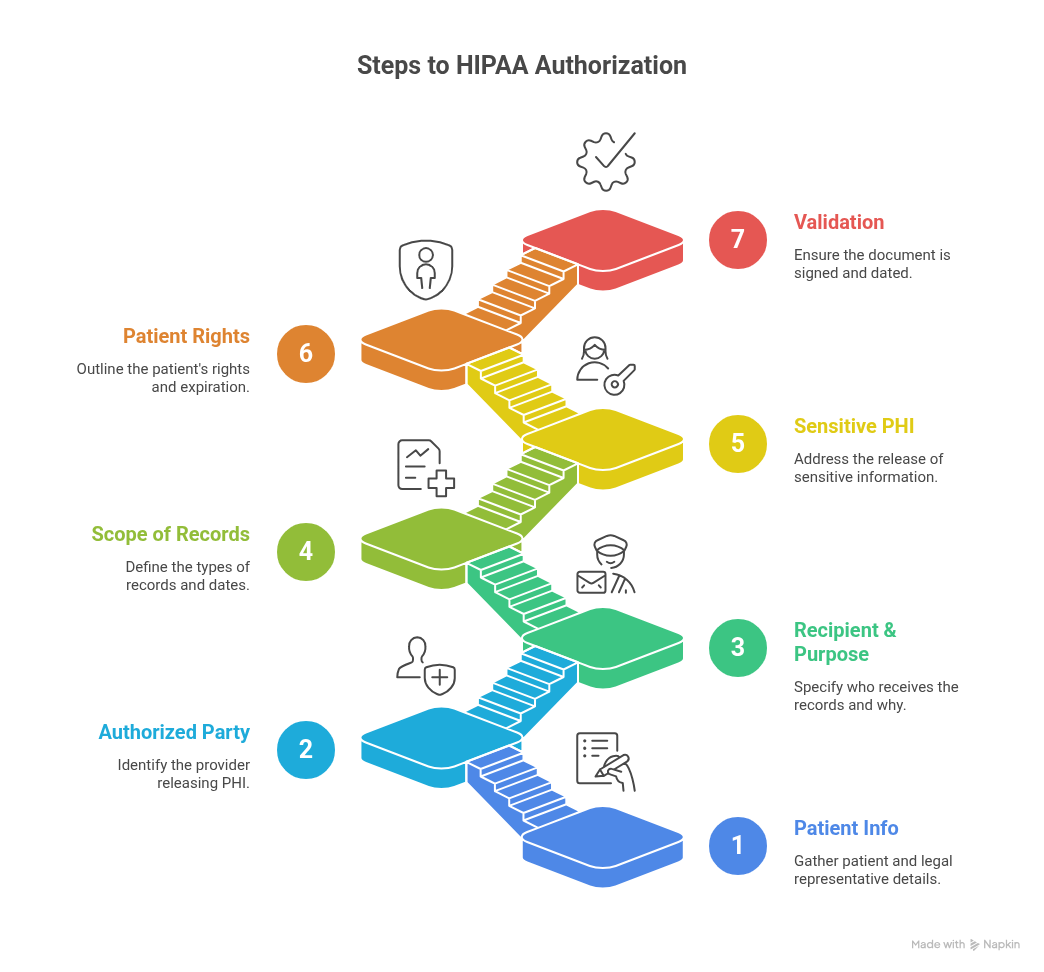
How to Complete a Medical Release Form
For administrative staff, the process of providing and receiving a complete, valid medical release form must be streamlined and auditable.
-
Selection: Select the correct, jurisdictionally appropriate Medical Release Form Template from the Wansom Library.
-
Pre-fill with AI: Use Wansom’s AI to pre-fill known patient demographics, the Recipient Law Firm’s details, and the litigation name/claim number.
-
Patient Review: The patient completes the highly specific sections: the scope of records, the dates of service, and explicitly initials any sensitive information waivers.
-
Signature & Validation: The patient (or legal representative) signs and dates the document. Wansom’s platform instantly validates that all mandatory HIPAA fields are complete before acceptance.
-
Documentation & Audit Trail: A copy of the form is provided to the patient, and the original is stored in the patient’s legal/administrative file. Wansom automatically records the form’s existence, scope, and expiration date in an immutable audit trail—essential for future compliance checks.
The traditional manual steps of form review and data transcription are replaced by immediate, automated compliance checking.
Medical Release Form Template Example
The core structure of a legally robust release form must clearly delineate the parties, the scope, and the patient's rights, adhering to the following structure:
Related to Blog: Best Practices for Documenting HIPAA Revocation of Authorization
Easier Medical Release Forms with Wansom
The complexities of state variations, sensitive data waivers, and the Minimum Necessary Rule make the generic online template obsolete for legal and compliance teams. Wansom is the only secure, AI-powered collaborative workspace designed to solve these specific legal and administrative headaches.
Here is how Wansom transforms your release form workflow:
-
Choose a Template from the Legal Library: Access Wansom’s comprehensive, legally vetted library, which includes specialized templates (e.g., California Mental Health Authorization, 42 CFR Part 2 SUD Release).
-
AI Fill and Contextualize: Instead of manual typing, upload your case file details or use the AI assistant to instantly populate the form with the recipient attorney's details, the case name, and the specific dates of injury. The AI ensures the scope is narrow enough to meet the Minimum Necessary Rule.
-
Dynamic State Law Adjustments: Simply select the jurisdiction (e.g., New York). The AI instantly adjusts the revocation language, confidentiality disclaimers, and required sensitive data checkboxes to comply with New York’s specific Mental Hygiene Law requirements.
-
Secure Finalization and Audit: Once signed, the form is stored with enterprise-grade encryption and automatically tracked in a centralized, immutable audit log. You have immediate, verifiable proof of consent, scope, and expiration date—essential for defending against claims of improper disclosure.
Trusted by leading legal firms for secure, compliant document automation, Wansom meets or exceeds all regional healthcare privacy and security standards (HIPAA, GDPR, etc.), ensuring patient data integrity and legal defensibility.
Conclusion: Securing Your Practice with Authority
In the arena of patient privacy, the Medical Records Release Form is the definitive legal document. Its accuracy is non-negotiable. Relying on manually completed or generic templates is a serious administrative and legal vulnerability.
For legal professionals and compliance teams, the strategic imperative is clear: adopt a dynamic, AI-enabled drafting system that guarantees adherence to the complex tapestry of federal HIPAA rules and stringent state-specific statutes. Wansom provides the secure, collaborative environment you need to automate these critical workflows, transforming the creation of a legally sound medical authorization into a fast, accurate, and audit-ready process.
Ready to eliminate legal risks and ensure every disclosure is valid and compliant?
Start customizing and downloading Wansom's AI-powered, state-compliant Medical Records Release Form template today.
Related to Blog: The Future of Legal Intake: AI-Powered Data Capture
FAQs About Medical Release Forms
-
What is a medical authority letter?
In most common contexts, a medical authority letter refers to a document that grants an individual (a Personal Representative) the legal authority to make healthcare decisions on someone’s behalf, including accessing medical information, especially when the patient lacks decision-making capacity. This authority is most frequently codified in a Durable Healthcare Power of Attorney (POA).
-
What is the difference between a medical liability release form and a medical release authorization form?
A medical liability release form (often called a waiver) is a document that limits a healthcare provider’s financial or legal liability for specified adverse outcomes related to a treatment or procedure. In contrast, a medical release authorization form grants permission for the disclosure of private health information. These are two distinct legal instruments used for entirely different purposes.
-
Can I create my own medical release form template?
While you are legally permitted to draft your own release of medical information form, it is generally recommended that legal and compliance teams start with a template that has undergone medicolegal review. The complexity of the six HIPAA elements, plus state-specific requirements (especially for sensitive data), makes it extremely difficult to create a compliant form from scratch without inadvertently omitting crucial protective language. Wansom templates are built on comprehensive legal analysis to mitigate this risk.